Preclinical Model Development
Preclinical models are crucial for evaluating the safety and efficacy of new therapies before human trials. These models, which encompass various in vitro and in vivo systems, play a vital role in mimicking human physiology and disease processes. Developing robust and reliable preclinical models is essential for accelerating the drug discovery process and reducing the risk of adverse events in human clinical trials. They allow researchers to test the potential of novel treatments in a controlled environment, providing insights into the mechanism of action, dosage, and potential side effects.
Different types of preclinical models, such as cell cultures, animal models, and organ-on-a-chip devices, each offer unique advantages and disadvantages. Careful consideration of the model's relevance to the human condition is paramount. For example, animal models, while offering insights into whole-body responses, may not always accurately reflect human responses. Choosing the appropriate model is critical for ensuring the validity and reproducibility of the results.
Clinical Trial Design and Implementation
Clinical trials are meticulously designed and implemented studies to evaluate the safety and efficacy of a new treatment or intervention in humans. A well-structured clinical trial protocol is essential for ensuring the scientific integrity and ethical conduct of the study. Robust statistical analyses are employed to determine the significance of the results. This process includes careful consideration of the study population, treatment arms, outcome measures, and data analysis methods.
Several key considerations are crucial for the successful execution of clinical trials. These include participant recruitment, data management, and regulatory compliance. Maintaining rigorous data quality and integrity throughout the entire trial process is vital for ensuring reliable results. Furthermore, careful attention to ethical considerations, such as informed consent and patient safety, is absolutely paramount.
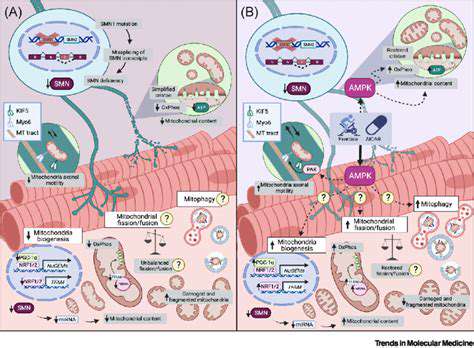
Translation from Preclinical to Clinical
Translating findings from preclinical models to clinical trials is a complex and crucial step in drug development. The success of this translation hinges on the careful consideration of factors such as the model's validity in reflecting human disease, the relevance of preclinical findings to human responses, and the potential for unforeseen side effects. Careful attention must be paid to extrapolating results from the preclinical setting to the complexities of the human body.
Significant discrepancies between preclinical and clinical findings can occur due to differences in species, physiological variables, and the inherent variability in human responses. These differences underscore the need for rigorous validation of preclinical findings in the clinical setting. Successful translation requires a comprehensive understanding of the limitations of preclinical models and the complexities of human biology.
The Future of Ophthalmic Drug Discovery: Emerging Trends and Opportunities
Personalized Medicine in Ophthalmic Drug Development
The future of ophthalmic drug discovery is increasingly focused on personalized medicine approaches. This involves tailoring treatment strategies based on individual patient characteristics, including genetic predispositions, specific disease subtypes, and even unique environmental factors. This personalized approach promises to significantly improve treatment outcomes by optimizing drug efficacy and minimizing adverse effects. Researchers are actively exploring biomarkers to identify patients most likely to benefit from specific therapies, leading to a more targeted and efficient drug development process.
By understanding the unique molecular profiles of individual patients, scientists can develop personalized treatment regimens that maximize the effectiveness of ophthalmic drugs and minimize the risk of side effects. This approach has the potential to revolutionize ophthalmic care, moving away from a one-size-fits-all approach to a more precise and patient-centric model. The development of sophisticated diagnostic tools and genetic analysis techniques further supports this burgeoning field.
Advancements in Drug Delivery Systems
Innovative drug delivery systems are crucial for enhancing the efficacy and safety of ophthalmic medications. Current challenges in delivering drugs to the eye include the delicate nature of the ocular tissues and the presence of the blood-ocular barrier. Novel approaches, such as targeted drug delivery systems, liposomes, and nanoparticles, are being explored to overcome these obstacles. These advancements aim to improve drug bioavailability, reduce systemic side effects, and enhance drug retention within the eye, ultimately leading to more effective treatments.
The development of sustained-release formulations, which gradually release the drug over a period of time, is another significant area of focus. These formulations can maintain therapeutic concentrations for longer durations, reducing the frequency of administrations and potentially improving patient compliance. Furthermore, the integration of nanotechnology into drug delivery systems offers the potential for precise targeting of specific cells and tissues within the eye, further optimizing treatment outcomes.
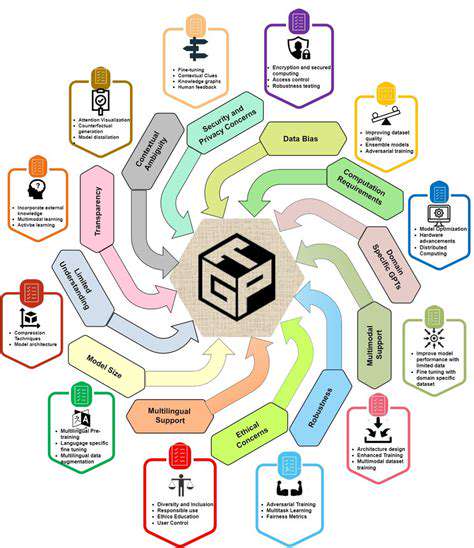
Artificial Intelligence and Machine Learning in Drug Discovery
Artificial intelligence (AI) and machine learning (ML) are rapidly transforming drug discovery across various therapeutic areas, including ophthalmology. AI algorithms can analyze vast datasets of genomic information, clinical trial data, and preclinical findings to identify potential drug candidates, predict their efficacy and safety profiles, and optimize drug design. This computational approach accelerates the drug discovery process, reducing time and cost associated with traditional methods. The use of AI in ophthalmology promises to unlock new avenues for developing effective and safe treatments for various eye diseases.
Ocular Biomarkers for Early Disease Detection
Identifying reliable biomarkers for early disease detection is crucial for improving treatment outcomes in ophthalmic conditions. Researchers are actively working to identify molecular signatures associated with different eye diseases. These biomarkers could be used to detect the onset of diseases like glaucoma or age-related macular degeneration at earlier stages, when interventions are most effective. Early detection allows for timely treatment, potentially slowing disease progression and preserving vision. The development of diagnostic tools based on these biomarkers could revolutionize the management of ophthalmic diseases.
Stem Cell Therapy and Regenerative Medicine
Stem cell therapy and regenerative medicine hold immense promise for treating various ophthalmic conditions. Stem cells, with their ability to differentiate into various cell types, could potentially repair damaged tissues in the eye and restore lost function. Research is focused on using stem cells to regenerate damaged retinal cells, treat corneal injuries, and potentially restore vision in conditions like macular degeneration. The potential of stem cell therapy to restore vision and treat previously incurable ophthalmic conditions is driving significant research in this field.
The Role of Gene Editing Technologies
Gene editing technologies, particularly CRISPR-Cas9, are emerging as powerful tools in ophthalmic drug discovery. These technologies allow scientists to precisely modify genes associated with eye diseases, potentially correcting the underlying genetic defects that cause these conditions. This approach holds great promise for treating inherited eye diseases, such as retinitis pigmentosa and Leber congenital amaurosis. The long-term implications of gene editing technologies in ophthalmology are vast and potentially transformative, offering new avenues for correcting genetic defects and restoring vision.